2019-11-30 17:09
作者 翻译:宁永忠
微生物学顾问应参与到ICU的每日查房中
A microbiologist consultant should attend daily ICU rounds
作者:J. Schouten、 G. De Angeli、J. J. De Waele
翻译:宁永忠 审阅:余跃天
Intensive Care Med https://doi.org/10.1007/s00134-019-05846-0
由于重症医学科(ICU)收治的患者中近50%伴有感染性疾病,因此,抗生素在此广泛应用并不令人惊讶[1]。同时,我们也可观察到由多重耐药(MDR)微生物引起感染的发病率在逐年增加,而抗生素的暴露是其促成因素之一[2]。
(Antibiotics are widely used in the intensive care unit (ICU); with approximately half of the patients diagnosed with an infection, this is not surprising [1]. In parallel, we are witnessing an increase in the incidence of infections caused by multidrug resistant (MDR) infections, in which exposure to antibiotics is a contributing factor [2].)
医院范围内的抗生素管理计划(antibiotic stewardship programs,ASP)已经实施,以减少抗生素暴露并改善患者预后。在涉及不同专业的多学科合作中,应用不同的干预措施可以帮助处方医生更好地作出抗生素决策。它可能包括提供指南、处方限制、审查和反馈[3]。
(Hospital-wide antibiotic stewardship programs (ASP) have been developed to reduce antibiotic exposure and improve patient outcomes. In a multidisciplinary approach involving different specialties, different interventions are used to assist prescribers in better antibiotic decision-making. This may include the provision of guidelines, formulary restrictions, review and feedback[3].)
ICU中广泛进行ASP会议[4],但其频率、持续时间和参与者各不相同——从每日开展的整个治疗小组针对每名患者治疗方案的会议,到每周开展的部分小组成员参与的疑难患者救治方案讨论。
(ASP meetings are widely used in the ICU [4] but the frequency, duration and its participants vary from daily meetings with the complete team discussing each patient to once-weekly meetings with part of the team to discuss the difficult to treat patients.)
我们一直提倡微生物学专业人员应经常参与ICU内病情讨论[5],且已有单中心的前后对照研究显示,临床医生和微生物学专业人员之间建立密切合作关系可以提高抗微生物治疗措施的实施。但目前尚无研究表明,微生物学专业人员参与日常查房与作为不同类型的“联络人”相比具有优势。不仅是在ICU,在其他病区亦是如此。此外,Lane等的系统综述[7]探讨了ICU患者救治中的有利及不利因素,并没有确定将“微生物学专业人员”(但确定了临床药师!)作为多学科团队合作的主角。
(Despite the presence of the microbiologist in ICU is frequently advocated [5], and studies have reported on improved antimicrobial practices after establishing a more closer interaction between clinicians and microbiologists in before-after studies in single-center studies [6], no study has formally demonstrated the superiority of a strategy with a microbiologist in daily rounds compared to different types of “liaisons” in ICU, nor in other settings. Furthermore, the systematic review by Lane et al. [7], which explored facilitators and barriers for patients care round in ICU, did not identify the “microbiologist” (but the pharmacist instead!) as leading character in multidisciplinary team rounds.)
不过,对抗微生物药物敏感性、局部生态学、宿主先前感染或定植MDR病原体的广泛认识,仍然是临床微生物学专业人员的核心能力之一,这对于ICU内正确的抗微生物治疗是基本的,也是必须的(表1)。
(Still, extensive knowledge on susceptibility patterns, local ecology, the importance of previous infections and colonization with MDR pathogens are among the core competencies of clinical microbiologists deemed essential for appropriate management of antimicrobial therapy in the ICU (Table 1).)
自从在医院引入ASP(通常是强制性的)以来,抗生素管理团队成员的负担越来越重,他们经常在没有额外工作人员或资金支持的情况下延长工作时间。对于现在需要将更多的临床推广工作与实验室实践相结合的微生物学专业人员而言,亦是如此。随着越来越多的部门要求每天/每周召开会议和连续增加工作时间,微生物学专业人员的工作量也在增加。因此导致了医务人员职业倦怠比以往任何时期都更为普遍,这一点不容低估。
(Since the (often mandatory) introduction of ASPs in hospital, an increasing burden has been placed upon Antimicrobial Management Team members, who have often extended their work without being provided additional workforce or funding. This is especially true for microbiologists who now need to combine more clinical outreach work with laboratory practice. As daily/weekly meetings and continuous out-of-hours service are requested by ever more departments, the workload for the microbiologist is increasing. In an era where physician burnout is more prevalent than ever before, this should not be underestimated.)
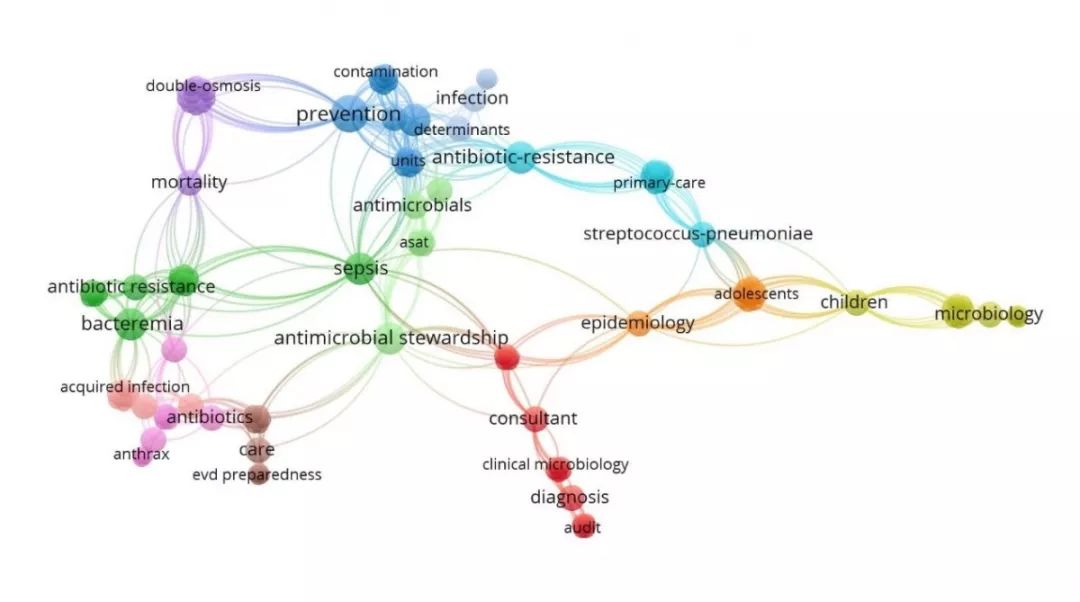
通过Vosviewer软件对于Web of Science 网站检索关键词“Microbiologist consultant”(微生物学咨询)所得的聚类分析图,提示研究热点及发展方向(余跃天制图并释义)。
即使重症医学科医生(intensivists)认为每天都有微生物学专业人员参与病情讨论是有价值的[5],但这种讨论的效率有时也值得怀疑:并非所有患者都存在感染相关问题或正在使用抗生素,而一旦讨论了感染相关话题,重症医学科医生可能会更关注于营养、呼吸机脱机或其他与感染无关但同样重要的问题。在此期间,微生物学专业人员似乎是在浪费时间。此外,出席会议的ASP团队其他成员也可能失去宝贵的时间。
(Even if daily presence of a microbiologist may be considered valuable by intensivists [5], the time efficiency of such meetings is obviously questionable: not all patients have an infectious problem or have antibiotics and—once the topic of infections is discussed—intensivists may linger on indefinitely about nutrition, weaning or any other non-infection-related (but equally important) problem during which the microbiologist is clearly wasting time. Moreover, other members of the ASP team present at the meeting may also be losing valuable time.)
随着快速诊断技术的引入[8],可以在数小时而不是数天内得到病原菌及抗生素敏感性结果。在某一固定时间召开的每日会议似乎已经过时,且会延缓抗微生物药物的最佳决策实施时间。此外,现代通讯技术和先进的电子医疗记录的发展,允许微生物学专业人员和ICU诊断小组之间通过其他方式进行互动讨论[9]。
(With the introduction of rapid diagnostics [8], establishing diagnosis of the causative pathogen and susceptibility patterns in a matter of hours rather than days, a daily meeting at a fixed moment seems obsolete and would essentially slow down appropriate antimicrobial decision making. Moreover, modern communication technology and advanced electronic medical records nowadays allow for other means of interaction between the microbiologist and the ICU team [9].)
那么,我们如何才能找到一种更有效、更省时的方法,将有价值的微生物学建议融入到现代ICU实践?
(So, how can we find a more efficient and less time-consuming way to integrate valuable microbiological advice into modern ICU practice?)
根据团队的经验、微生物学专业人员参与的可能性和特定时刻的需求而定制特定方法是可行的。对成立时间较短的ASP团队而言,整个团队的日常会议可能会非常有价值。但随着团队整体经验的增长,抗微生物药物处方条目规范,实验室处于全天24h工作制,且配有微生物学专业人员随时待命以便将微生物学结果最快速地传达给ICU小组。在这种情况下,每次会议病情讨论未必一定必须。一个成熟的ASP团队,应利用会议来增强抗生素及相关知识和策略,以及引入新的概念或讨论生态学等。在那个阶段,许多抗微生物药物处方都包含在指南和标准实践中,对此,每日查房团队已经非常熟悉了。
(Based on the experience of the team, the availability of the microbiologist and the needs of the unit at a specific moment in time, a unit-tailored approach can be preferable. In recently started ASP teams, daily meetings with the whole team may be very valuable, but, as experience of the team grows, antibiotic therapy is settled in clear local guidelines, laboratory is 24/7 and a microbiologist is available on call for the most rapid communication process of microbiology results to ICU team-the role of daily meetings may change. In a mature ASP team, meetings should be used to reinforce knowledge and strategies as well as to introduce new concepts or discuss ecology, etc. At that stage, much of the antimicrobial prescriptions are covered by guidelines and standard practices which are now very familiar to the bedside team.)
我们仍然相信,面对面的接触对于实施良好的抗微生物药物管理至关重要。虽然使用现代信息技术解决方案的日常即时反馈现在是可行而且有效的,但出现如下情况我们仍期望在ICU内可以得到微生物学专业人员的专业建议(并非ICU每日查房都需要)(表1):
(We remain convinced that face-to-face contact is essential for implementation of good antimicrobial stewardship. While day-to-day immediate feedback using modern information technology solutions is now feasible and effective, we must keep seeing the microbiologist in our ICU in person on a regular basis (but not necessarily daily during ICU rounds) to (Table 1):)
•讨论ICU中与治疗耐药菌相关的处方决策或改变。
(Learn about our prescribing patterns related to (changing) resistance patterns in our ICU unit.)
•讨论ICU中(快速)诊断方法的新进展,及其在相关抗微生物药物管理原则方面的作用。
(Learn about new developments in (rapid) diagnostics and their effect in relevant antimicrobial stewardship principles in ICU.)
•协助解释相关微生物学检查结果或减少不必要的检查。
(Assist in interpretation of results or in reducing unnecessary testing.)
ICU中临床微生物学的核心领域 | 频率 | 活动 |
辅助医生进行诊断、经验治疗 | 每天 | 电话随时联系,就结果快速交流、提供咨询,开发实践指南 |
辅助解释结果 | 每天 | 报告提示污染/定植,选择性报告抗微生物药物敏感性,教学会议 |
避免不必要的检查 | 每天 | 教学培训,核查反馈,电子信息置入 |
辅助正确的微生物学标本采集、时效性 | 每天 | 电话随时联系,实践指南,对新的和进展性的诊断检查技术进行教学培训 |
辅助选择最优的靶向抗生素、正确的疗程 | 每天到每周 | 定期开会,电话随时联系,选择性报告抗微生物药物敏感性,计算机辅助决策系统,开发实践指南 |
基于感控目的,提供耐药微生物的累积性检测数据 | 每3月,或6月-1年 | 医院内部网络,打印版,教学会议 |
易化感控措施 | 每天 | 电话随时联系,实践指南,教学会议 |
而另一面,微生物学专业人员也必须定期参与到ICU的疑难病例讨论中,以提高其综合会诊技能。定期与重症医学科专家互动,将促使这一项内容更好实施。
(Conversely, microbiologists must be exposed regularly to the clinical complexities in ICU to improve their integrative consultation skills and regular interaction with intensivists will facilitate this.)
我们提倡采纳与临床微生物学专业人员和其他ASP团队成员会晤的替代计划,如下所示:
(We advocate the adoption of an alternative scheduling of appointments with clinical microbiologists and other ASP team members as below:)
•每周一次,与微生物学专业人员讨论临床疑难患者的诊治方案。
(Once weekly clinical round in which difficulty-to-treat patients are discussed with the microbiologist.)
•每3-6个月进行一次反馈会议,提供关于正确处方依从性的数据(使用ICU抗微生物药物处方的相关质量指标,如指南依从率、适当的疗程和PK-PD),并审视医院范围内MDR病原体的出现情况。
(Once per 3-6 months feedback session with data on adherence to appropriate prescribing (using relevant quality indicators for antimicrobial prescribing in ICU such as guideline adherence, appropriate duration and PK-PD) and an oversight of hospital-wide emergence of MDR pathogens.)
•在感染性疾病暴发或流行期间,需要更频繁(甚至每天)召开会议,以加强密切合作,并强化感染控制措施。
(More frequent (and even daily) meetings during outbreaks or epidemics requiring close collaboration and with need for intensified infection control measures.)
总之,以微生物学知识为基础,微生物学专业人员在ICU感染管理中的重要性是毋庸置疑的。然而,在现代通讯时代,一旦ICU的抗微生物药物管理计划完全建立起来,可能就不再需要微生物学专业人员每天面对面的查房了。我们一方面支持使用连续数字化的微生物学支持和建立ICU适应性指南,另一方面支持在真正需要微生物学专科建议时,采用更灵活的面对面方法。每周7天24小时全天候提供(随时待命)微生物学专业咨询来验证诊断检查对于快速改变治疗方法而言,至关重要。我们确实相信,有必要举行结构性的(不是每天,而是每周或每月)会议,以保持双方的一致。
(In conclusion, the importance of a microbiologist with his/her knowledge based in the management of ICU infections is undisputed. However, in this era of modern communication tools, physical presence of a microbiologist at a daily face-to-face ward round may not be needed once an ICU antimicrobial stewardship program is fully established. We support the use of continuous digital microbiological support and established ICU adapted guidelines on one hand and a more flexible face-to-face approach when dedicated advice is really needed. 24/7 availability of an (on call) microbiologist to validate rapid diagnostic testing is essential to allow for fast change of therapy. We do believe that structural (not daily but weekly or monthly) meetings are warranted to keep both parties aligned.)
译者按:
一方面,欧洲(作者是荷兰、意大利、比利时)的ICU与微生物学的互动,深入而丰富,远远超过了我们的想象。和循证医学临床实践指南一样,我们还在未证之先,他们已经是既证之后。也好吧,我们一面建构一面解构,骨感的现实成就我们复合的理念,“瞻前顾后”交辉我们渴望的眼眸!
一方面,能够看到欧洲临床医生对微生物学无缝嵌入的思考、尊敬、现实、弹性……医学既是技术,也是理念,更是团队合作互相成就,也是与时俱进消长融通!合作与圆融才是人类的本质。马克思谓:人是一切社会关系的总和。而医生纳入了微生物学观念,恰是完成了医学修炼的一阶、一节,可作一结、一嗟!
一方面,弱弱地说,题目是余医生铁定。我不敢用“顾问”一词。(●’◡’●)
参考文献
1. Vincent JL, Rello J, Marshall J, Silva E, Anzueto A, Martin CD, Moreno R, Lipman J, Gomersall C, Sakr Y, Reinhart K, EPIC-II Group of Investigators (2009) International study of the prevalence and outcomes of infection in intensive care units. JAMA 302:2323–2329. https://doi.org/10.1001/jama.2009.1754
2. Timsit JF, Bassetti M, Cremer O, Daikos G, de Waele J, Kallil A, Kipnis E, Kollef M, Laupland K, Paiva JA, Rodríguez-Baño J, Ruppé É, Salluh J, Taccone FS, Weiss E, Barbier F (2019) Rationalizing antimicrobial therapy in the ICU: a narrative review. Intensive Care Med 45:172–189. https://doi.org/10.1007/s00134-019-05520-5
3. Charani E, Cooke J, Holmes A (2010) Antibiotic stewardship programmes—what’s missing. J Antimicrob Chemother 65:2275–2277. https://doi.org/10.1093/jac/dkq357
4. Kollef MH, Bassetti M, Francois B, Burnham J, Dimopoulos G, GarnachoMontero J, Lipman J, Luyt CE, Nicolau DP, Postma MJ, Torres A, Welte T, Wunderink RG (2017) The intensive care medicine research agenda on multidrug-resistant bacteria, antibiotics, and stewardship. Intensive Care Med 43:1187–1197. https://doi.org/10.1007/s00134-017-4682-7
5. Wilson L, Dempsey G (2007) Medical microbiology ward rounds in critical care. Crit Care 11:P75. https://doi.org/10.1186/cc5235
6. Arena F, Scolletta S, Marchetti L, Galano A, Maglioni E, Giani T, Corsi E, Lombardi S, Biagioli B, Rossolini GM (2015) Impact of a clinical microbiology-intensive care consulting program in a cardiothoracic intensive care unit. Am J Infect Control 43:1018–1021. https://doi.org/10.1016/j.ajic.2015.04.200
7. Lane D, Ferri M, Lemaire J, McLaughlin K, Stelfox HT (2013) A systematic review of evidence-informed practices for patient care rounds in the ICU. Crit Care Med 41:2015–2029. https://doi.org/10.1097/CCM.0b013e31828a435f
8. Decousser JW, Poirel L, Nordmann P (2017) Recent advances in biochemical and molecular diagnostics for the rapid detection of antibiotic-resistant Enterobacteriaceae: a focus on β-lactam resistance. Expert Rev Mol Diagn 17:327–350. https://doi.org/10.1080/14737159.2017.1289087
9. Curtis CE, Al Bahar F, Marriott JF (2017) The effectiveness of computerised decision support on antibiotic use in hospitals: a systematic review. PLoS One 12:e0183062. https://doi.org/10.1371/journal.pone.0183062

翻译:宁永忠
审阅:余跃天